In Part 1 we spent some time unpacking what we actually mean when we say ‘Ultra Processed Food’ (UPF), how it is defined and categorised, and how that definition is vague and includes a huge variety of pretty disperate foods. [Read it here if you haven’t already]
Today we’re going to get a little deeper into the science - what do we know? And what are we still figuring out?
And the answer to those questions is not much, and a lot, respectively.
It’s estimated that around 56.8% of food eaten in the UK is ultra processed. When we split the UK population into five groups - the bottom group, representing the lowest intake of UPFs, eat around 34.9%, and the group representing the highest intake eat around 78.1% UPFs.
Higher consumption of UPFs has been linked to an increased risk of adverse health outcomes, including heart disease, high blood pressure and metabolic syndrome, some cancers, depression, irritable bowel syndrome, adolescent asthma and wheezing, frailty, and overall mortality (death).
This, quite reasonably, causes people to panic. And it isn’t helped by anxiety-inducing headlines like this Time article ‘Why Are Processed Foods So Bad for You’, and this in The Times ‘Britain's Diet is More Deadly Than Covid’ and this WaPo piece detailing what we should eat instead of UPF. But instead of being thoughtful musings on how to repair a broken food system, they’re perfect examples of writers uncritically regurgitating university press releases.
Upfront, my argument is not that we don’t need to change the food system. My argument is that the headlines have leapfrogged science, allowing people in places of power and privilege to create fear and shame about the food we eat. This keeps us focused on food as the issue, rather than the social, political, and structural forces that shape our lives and our experiences of wellbeing.
Let’s take, for instance, the recent Times dumpster fire by Henry Dimbleby (objectively, not a Science Dude). In it, he tacitly implies that diabetes is the result of a diet high in UPFs. He provides not one shred of evidence for this. Yet, a 2021 meta-analysis - one of the biggest, most robust studies to date of the literature on UPF - found ‘no significant associations with hypertension, hyperglycaemia or hypertriacylglycerolaemia.’1 Hyperglycaemia is elevated blood sugar levels - persistently high blood glucose levels are characteristic of diabetes (due to either insufficient insulin, or insulin not working properly). Even research conducted by Dimbleby’s mate, Tim Spector, found that, 50% of the variation of blood glucose is genetically determined (even if his predictive modelling is about as effective as a coin flip lol).
The evidence on UPFs is not as clear cut as the headlines make us believe. And the evidence and headlines alike are steeped in trenchant anti-fatness; a set of underlying assumptions, beliefs, and attitudes that lead to the dehumanisation of bigger bodies. Anti-fat bias in and of itself contributes to many of the outcomes presumed to be caused by higher weight; depression, metabolic disease, type 2 diabetes, heart disease, and early death. Much in the same way that experiencing any form of oppression threatens the wellbeing and safety of our bodies.
The moral panic about UPFs, has a lot less to do with health per se and more to do with unexamined anti-fat bias. Dimbleby’s assertions that UPFs are the common thread between fat2 bodies and disease neglect to consider the impact of systemic discrimination; the cumulative impact of being denied access to healthcare, being ostracised from public spaces, having a war waged on your body simply for existing.
It is so much easier to blame food than to look at this, isn’t it Henry?

As we consider the literature on UPFs, we cannot separate it from the researchers’ biases. The false belief that weight in and of itself leads to worse health. The false belief that even if weight did cause poor health, that we had a permanent solution for weight loss. The false belief that BMI predicts health outcomes in a linear way. And the perpetual denial of fat folks’ lived experiences in their own bodies.
Understanding that the literature on UPFs is steeped in this bias can help orient us. How much of our disgust of ultra-processed foods is thinly veiled disgust towards fat people?
Ok, let’s go.
While the concept of UPFs has blown up in nutritional sciences in the last ten years, ten years is not a long time in science terms. This means that the type and amount of evidence we have on UPFs is limited. Nutrition research is also notoriously difficult to conduct - it’s extremely hard to tease apart the effects of diet from other life stuff. The vast majority of the studies we have on UPF are observational; this means we can’t deduce cause and effect. We can only say whether or not there are associations between two variables (in this case amount of UPF eaten and disease outcomes). We cannot say that UPFs cause a particular disease.
I spoke to , Professor of Economics at Brown University (but you may know her better from or from her books such as Crib Sheet). This is what she had to say about observational studies in nutrition research:
‘I think this is reflective of a very broad issue with research on nutrition, which is that diet is extremely difficult to separate from many other aspects of behaviour and from demographics. So it's really, really hard to isolate individual pieces of diet or individual foods and be able to say in some causal sense, this is the thing that is causing differences in health. So it's absolutely right that if you showed me two people's diets and you said, which of these people do you expect to, on average, have less heart disease, I could probably tell you this is the diet that I think would be associated with lower risk of heart disease. But it's associated with, it's not causal, because, on average, people who have a diet with more vegetables and more whole foods are also better educated, have better access to healthcare, have more income, more resources, all kinds of other stuff that also is positive.’
It’s extremely difficult in nutrition research to tease out what is caused by the food itself versus the conditions that people are living in that contribute to them eating a particular way. And what is attributable to the diet per se, versus the conditions we live in.
Let’s look at a recent, highly publicised study on the relationship between cancer and UPFs, when we look at the characteristics of the people in the study - the group who ate the highest number of UPF were different on almost every measure possible than the group who ate the lowest amount of UPFs. The people who had the highest intake of UPFs were older, had a stronger family history of cancer, exercised less, had lower household income, lower educational attainment, and were more likely to live in the most deprived neighbourhoods. Their diets also differed significantly in terms of key aspects of their diet - total energy, salt, carbohydrate, and total fat intake.3
And while the researchers try their best to adjust for this in their statistical methods - you can’t account for everything. Important variables such as racism, adverse childhood events, trauma, chronic stress, ableism, and of course, anti-fat bias - just to name a few - are missing.
Here’s again:
‘There's two problems. So one is the sort of residual confounding, or economists call it omitted variable bias. But that's the idea that there are characteristics of people like ACEs [adverse childhood experiences]... even detailed information about resources is mostly not controlled for in these studies. That, and those things, if you could see them, would relate to both dietary choices and outcomes and therefore they are biassing the results. So that's kind of one problem.’
She goes on:
‘And then there's a second problem, which is reverse causality… which is that it may actually be the case that there potentially is some causal relationship, but it goes the other direction. So instead it's kind of something else, some way in which the health experience is driving differences in dietary choices.’
It’s not unreasonable to infer that instead of UPFs causing people to get sick, that people who are sick rely more heavily on UPFs. Perhaps they are more convenient when attending hospital appointments, or they’re what’s affordable when living on benefits, or they’re more accessible to people with disabilities. In reality, the relationship is far more complicated than X → Y, (and it most likely goes both ways) but this is never the way it is reported in the media.
This is particularly important when looking at cross-sectional studies, where researchers are only looking at a snapshot in time. A single data point can tell us about prevalence (i.e. the estimated amount of UPFs in the diet or number of people in the sample with a given disease), but, again, it cannot tell us about the direction of a relationship. Cross-sectional studies make up around half of the high quality studies we have on UPFs.
To overcome some of the limitations in observational studies, researchers perform meta-analyses. These are statistical analyses performed on the pooled data of multiple studies - they are more powerful than looking at any individual study on its own. There are only a handful of these kinds of studies on UPFs - one of the most comprehensive was published in the British Journal of Nutrition in 2021.4 They identified a total of 23 studies to include in their analysis; 10 cross-sectional studies, and 13 cohort studies.5 I’m going to focus on the cohort study analysis because these are considered to be the more robust of the two study designs. The researchers found that compared to the lowest intake of UPF those consuming the highest amount of UPFs in their diet had a 25% higher risk of death, 29% higher risk of cardiovascular disease, 20% higher risk of depression, and 34% higher cerebrovascular disease (e.g. dementia).
Now, I know this sounds scary. Really scary. Which is why we have to go a little deeper than just reporting the headlines. What this analysis is telling us is the relative risk of eating more UPFs. So, relative to the people who eat the least UPFs, people who eat the most UPFs have a 29% higher risk of cardiovascular disease. BUT, we don’t know what the total or absolute risk is and just looking at the relative risk gives a far bleaker picture.
We don’t know what the baseline risk of cardiovascular disease is - but let's say for argument's sake (and simplicity of numbers) that it’s 10%. A ~30% increase on 10% baseline risk changes the risk from 10% to 13%. So, the absolute risk hasn’t changed much at all. This is not to say that there is no impact of ultra-processed foods on health - clearly there is. This is about keeping that risk in perspective.
We also don’t really know what constitutes a ‘high’ level of UPF consumptions vs a ‘low’ one as each of the studies included in this analysis used different cut offs for what counts for each. For example - the ‘low’ intake ranges from 6.5% of total energy intake all the way through to almost 18% of total daily energy intake from UPFs. On top of this, the tools we tend to use in nutrition to measure how much of any given food is in someone’s diet were never designed to capture foods according to NOVA classification. Given how subjective NOVA is (and how it’s definitely open to interpretation), we can’t even be sure that we’re accurately measuring the number of UPFs in someone’s diet anyway!
This leads to discrepancies in estimates of how much UPF is in the UK diet - the 56.8% value I have quoted already is based on sales data, not on food records. But this is the figure that I see referenced constantly. Without question. The much publicised Lancet cancer paper from earlier this year put the average UPF consumption at 22.9% with a range of 9.2% - 41.4%. These are wildly different numbers - but it’s the scary sounding one that the media hone in on.
Coming back to the level of risk - there are still problems with interpreting the results of just a handful of studies. Although the meta-analysis in question looked at 13 studies altogether, only five measured overall risk of death, three looked at cardiovascular disease risk, and two looked at cerebrovascular disease. This again highlights the lack of high quality studies in this area. The authors themselves state:
‘These results, although reporting interesting and useful data to formulate a hypothesis, must be carefully interpreted due to the low number of subjects and studies investigated.’
They go on to say:
‘The number of studies included was limited, especially for individual outcomes, and does not allow us to be sure that the results obtained are completely reliable but is sufficient to hypothesise the nature of the association that must then be tested in intervention studies for validation’.
Unlike observational studies, intervention studies are experiments where scientists alter variables between a control and experimental group. This is an important step in the scientific method, and helps increase our confidence that relationships aren’t down to chance or noise from residual confounding variables that Emily discussed earlier.
The gold standard of these studies is a double-blind placebo controlled trial.
There are no double-blind placebo controlled trials on UPFs.
We only have one randomised control trial (RCT) to date and it’s unblinded, meaning the researchers and the participants were both aware of the experimental conditions - whether they received a diet of UPF or ‘whole’ foods. Granted, it’s almost impossible to do these kinds of trials in nutrition research (unlike drug trials where you can give people a placebo pill).
When this study was first published, in 2018, I was studying my PGDip in Eating Disorders and Clinical Nutrition at UCL. The way lecturers were talking about this study, you’d have thought they had discovered a new vitamin or solved global malnutrition or something. It’s considered a really BFD in nutritional sciences. But, again, people seem to only be looking at the headlines - even other scientists and researchers! So, let’s not be those people. Let’s look a little closer.
The study in question, Ultra-Processed Diets Cause Excess Calorie Intake and Weight Gain: An Inpatient Randomized Controlled Trial of Ad Libitum Food Intake was led by Kevin Hall (a BFD Science Guy) and his team at the National Institutes of Health in the US. They recruited 20 adults (average age 31 years old) and provided all their food and drink for a month (they actually lived at the NIH - sweet gig if you can get it).
The participants were split into two groups. The first group ate what the researchers called ‘unprocessed’ foods (which is confusing because according to NOVA classification, they would be considered processed, but I digress). The second group ate a diet of UPFs. They followed their allocated diet for two weeks, and they were allowed to eat as much as they wanted. The two diets: unprocessed and ultra processed were matched in terms of nutritional value - so although the degree of processing differed, they were more or less the same in terms of calories, sugar, fat, fibre, vitamins and minerals.
After two weeks on one diet, the researchers swapped them to the other diet for another two weeks. During both diets they measure things like changes in weight, the speed at which they ate the respective diets, how much they ate at each meal (measured in calories), familiarity and palatability of the meals, their energy expenditure and so on. They also measured several biomarkers - such as blood glucose and cholesterol - using blood tests.
The researchers' results are presented in this graphical abstract. This is the science equivalent of a tl;dr. And this is pretty much the only part of the paper that gets reported on.
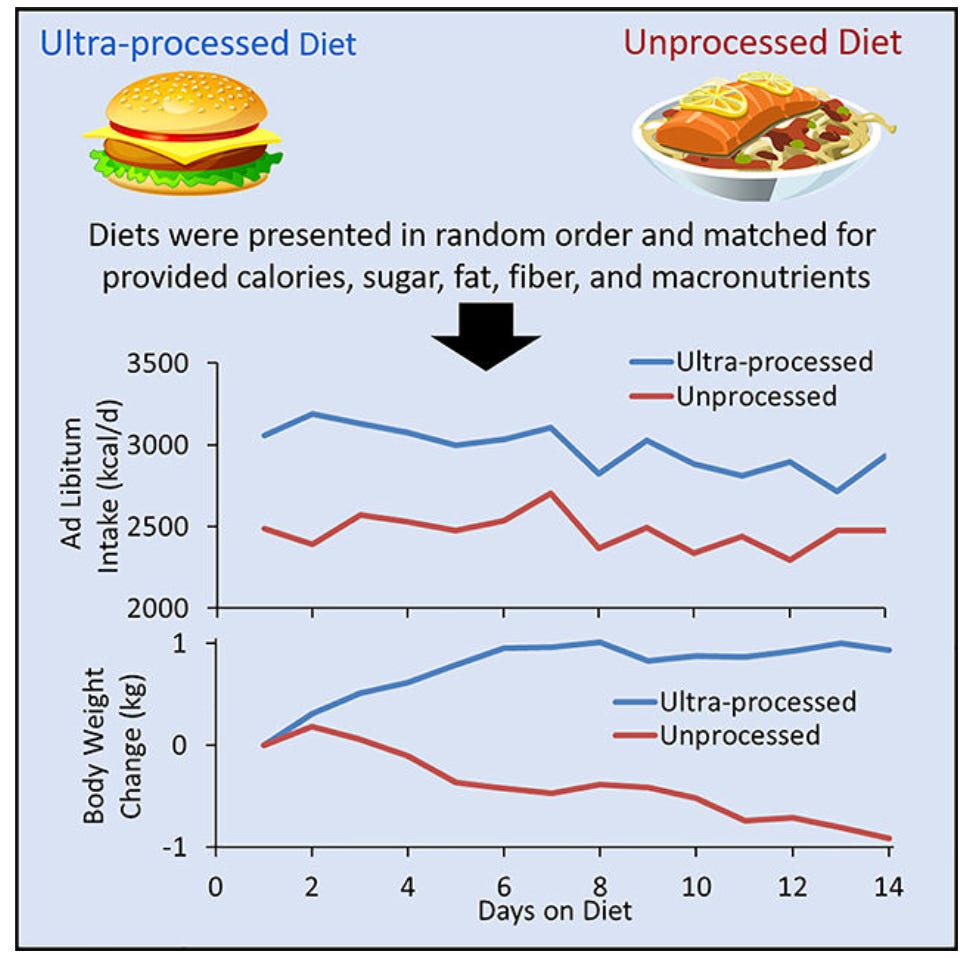
What this tl;dr shows is that, on average, people who were eating the UPF diet ate around 500kcal more per day than the people on the unprocessed diet. And on average, people eating the ultra-processed diet gained 0.9kg, while those on the unprocessed diet lost 0.9kg. The number of calories people were eating was highly correlated with weight gain (doy!). They also reported that eating rate was faster for the UPF - whether measured by grams per minute or calories per minute. Ghrelin - a hormone that is associated with hunger - decreased during the unprocessed phase compared to baseline.
This resulted in many a fear-mongering headlines about how UPFs will make you ‘eat more’ and how they are responsible for the ‘ob*sity epidemic’. But if we go beneath the headlines, we see a different picture.
We see that 50% of weight gain and loss was attributed to water weight. We see that there was, as one researcher put it - a ‘rapidly weaning effect on energy intake’ - indicating that, although energy intake was higher at the beginning of the UPF diet period, the trend line was going down. If we extended the study out beyond the TWO WEEKS it was conducted for, might we have seen that effect stabilise over time? We also see that there’s no difference in blood glucose and insulin response between the two diets - in either direction! (Suck it, Dimbleby). We see that the researchers are deeply invested in a narrative that fatness is pathology, rather than a function of human diversity in a world where we (mostly) have enough to eat, or one of the 100+ factors that determine a person’s weight.
What I find really, really interesting about this study is that in many ways it says the OPPOSITE of what people believe to be true about UPF. A common refrain is that these foods are manipulated by the food industry to be so irresistible and delicious that you cannot help yourself. Even those with the most resolve and steely willpower are defenceless against Double Stuff Oreos or Gregg’s sausage rolls. But in this study, the participants rated the palatability of the ultra-processed foods as the same as the unprocessed foods.6 This is a very different picture, throwing a kink in the narrative that people have no self-restraint in the face of these foods.

That said, we can’t draw firm conclusions from this study, because it was only two weeks long! And it only included 20 people! And it was unblinded! And even the people who eat the most UPF don’t eat 100% UPF. And. And. And.
This paper tells us virtually nothing. As one critic of NOVA said ‘[these results] can be entirely explained by more conventional and quantifiable dietary factors, including energy density, intrinsic fiber, glycemic load, and added sugar’.
If we weren’t so deeply invested in the narrative of fatness as pathology, would this study have been given as much airtime? Would we have been so uncritical about its findings?
As I said, our food system is broken. But we are kidding ourselves if we think the problem begins and ends with food. In part 3, we’ll explore some of the reasons - for better or worse - that we depend and rely on UPFs to feed ourselves.
ICYMI last week: The Truth About Ultra Processed Foods - Part 1

- Nourishing Myself with Laxmi Hussain
- Sweet Little Lies
- Fundamentals: Why Teaching Kids That Food is ‘Healthy’ Can Backfire
These studies are not flawless though, more on that later. ↩
I’m using the word fat as a descriptor, not as an insult in the spirit of fat liberation. ↩
The tools we use to quantify diets - namely food frequency questionnaires and food diaries - predate the development of NOVA. This means they weren’t designed to measure NOVA categories and, as far as I know, haven’t been validated against this system. This is on top of the existing issues we have with dietary assessment - mainly that it’s just hard to remember what you ate yesterday, let alone a week, a month, or a year ago (sometimes it’s even longer than that!). It’s by no means the biggest issue with this research, but it’s an important point that I couldn’t figure out where to fit in so it’s going in this footnote. ↩
In addition to the one I reported here - there is a meta analysis that claims to measure the dose-response relationship between the amount of UPF consumption and type 2 diabetes risk i.e. how as the amount of UPF in the diet increases, so does the risk of type 2 diabetes. In fact, out of the 18 studies they included in their analysis, 14 of them measured processed red meat intake, and one looked at beverages, and only three measured ultra-processed food using the NOVA system. One interesting finding is that there was no impact on diabetes risk consuming a moderate amount of ultra-processed meats, but there was when consuming a diet high in these foods. The second is this study showing a dose-response in mortality risk for 10% change in ultra-processed food consumption in daily intake, but has similar issues as the one I included here. ↩
Cross-sectional studies are where researchers follow a group of people over time. They are considered more robust than cross-sectional studies, but still have many of the same issues of confounding, among other limitations. ↩
(Side theory: A major part of the reason why these foods can feel irresistible is because they are restricted - if not physically, then subconsciously. A big part of why they are restricted is because people are shamed for eating them. Although the researchers tried to control for this - it was an indirect measure - they say there was no difference in familiarity between processed and UPFs. They infer that people were not restricting themselves, and therefore this wasn’t a cause for ‘disinhibited’ eating that could account for the differences in eating rate. However, measuring familiarity with a food is not the same as measuring restrained eating, nor is it a measure of perceived shame or guilt when eating these foods. Indeed, research on non-diet approaches has shown that people who don’t restrain their food are less influenced by external forces such as marketing and product placement in supermarkets).
With thanks to Jennie Agg of Life, Almost for editorial support on this series. ↩
